Postmenopausal women undergo bilateral oophorectomy whereas one or both ovaries are preserved in premenopausal women. That includes stage I cervical cancer and more specifically stage IA2 and IB1.

During the 20102013 period 2461 women with data in the National Cancer Database underwent radical hysterectomy for stage IA2 or IB1 cervical carcinoma and met the inclusion criteria.
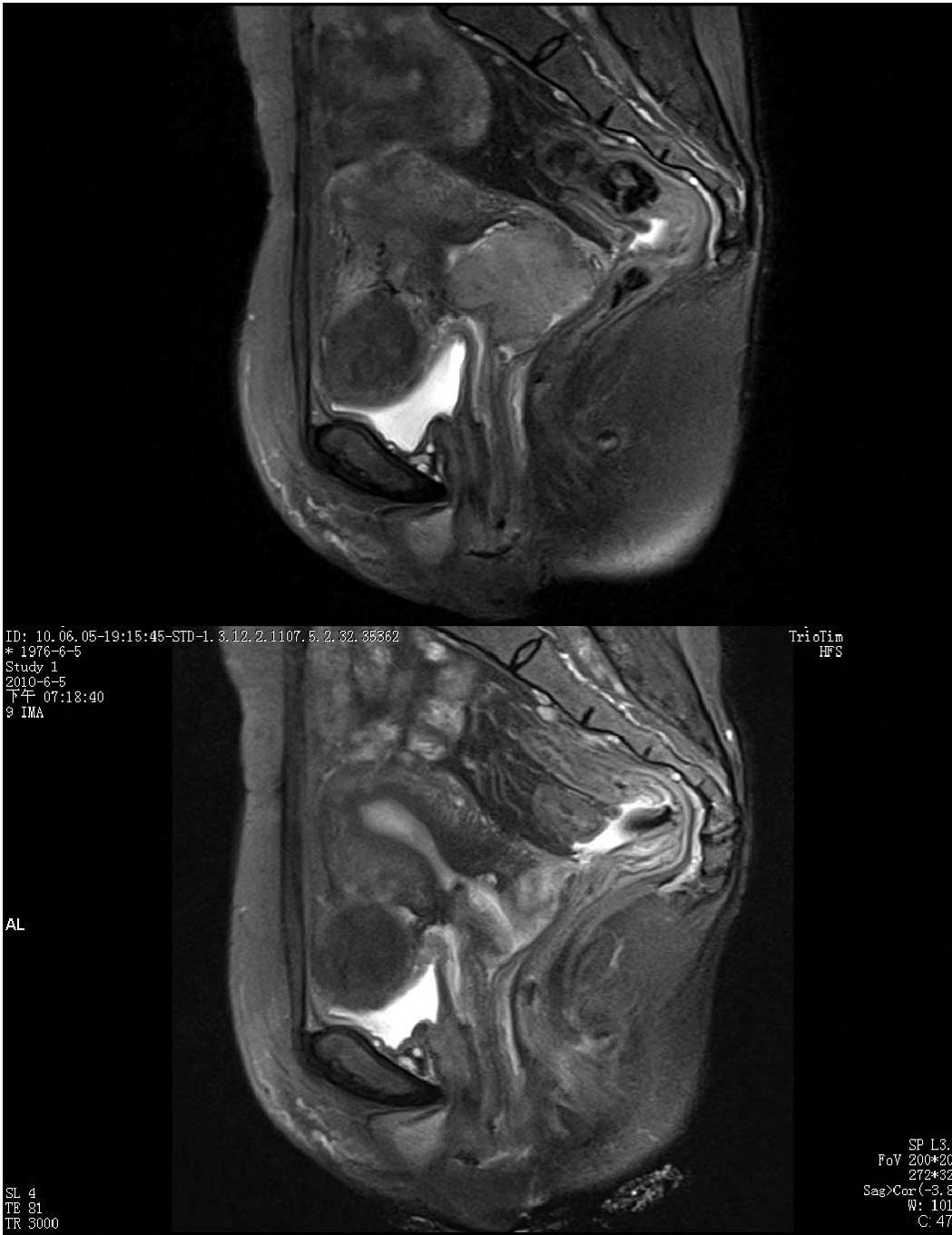
Stage 2 cervical cancer hysterectomy. Surgery options after birth for early-stage cancers include a hysterectomy radical trachelectomy or a cone biopsy. If the cancer is stage IB or higher then you and your doctor must decide whether to continue the pregnancy. If not treatment would be radical hysterectomy.
Simple hysterectomy the cervix and womb are removed and in some cases the ovaries and fallopian tubes are too. Only appropriate for very early-stage cervical cancers. Radical hysterectomy preferred option in advanced stage 1 and some early stage 2 cervical cancers.
The cervix womb top of the vagina surrounding tissue lymph nodes fallopian tubes and sometimes ovaries are all removed. Stage 1 In this stage the cancer has spread metastasized from the cervical lining into the deep cervical tissues. However is still contained in the uterus.
Stage 2 In cervical cancer stage 2 the cancer has spread outside the uterus to nearby regions such as the tissues surrounding the cervix or the vagina. A radical hysterectomy is the standard treatment for early-stage cervical cancer. That includes stage I cervical cancer and more specifically stage IA2 and IB1.
Often these patients are younger between ages 20 and 40. Surgery is not the standard. Hysterectomy for cervical cancer Hysterectomy is the usual treatment for early stage cervical cancer.
A hysterectomy involves removing the womb and cervix and occasionally the fallopian tubes and ovaries. A hysterectomy is only suitable for women with very early-stage cervical cancer stage 1A1. Surgery for invasive cervical cancer.
Procedures to treat invasive cervical cancer are. Hysterectomy simple or radical Trachelectomy. A simple hysterectomy removes the uterus both the body of the uterus and the cervix but not the structures next to the uterus parametria and uterosacral ligaments.
During this stage cancer cells have been found deeper within your cervix but the cancer cells havent spread to other structures. At this stage cancer cells have been found in your. If you had a total or radical hysterectomy as a treatment for cancer or pre-cancer your doctor may still recommend regular tests to check for cancer.
Even though your cervix is gone you may still be at risk for cancer in your vagina or nearby tissue. If your total or radical hysterectomy was for another condition other than cancer you should not be at risk for cervical cancer in the future but check with your doctor. The cancer has spread into the upper part of the vagina or the tissues next to the cervix.
Stage 2 can be further divided into. The cancer has spread into the upper part of the vagina. The cancer is no larger than 4cm.
The cancer is larger than 4cm. The cancer has spread into the tissues next to the cervix. During the 20102013 period 2461 women with data in the National Cancer Database underwent radical hysterectomy for stage IA2 or IB1 cervical carcinoma and met the inclusion criteria.
The standard treatment is surgery called a total hysterectomy to remove the uterus and cervix. Cancer is in the outer layer of your uterus or the fallopian tubes and ovaries. Stage II stage 2 cervical cancer.
Stage II cervical cancer means that the cancer has grown beyond the cervix and uterus but has not reached the walls of the pelvis or the lower part of the vagina. In this stage of cervical cancer the disease has not spread to lymph nodes or distant sites. 1 Nov 2005 Read the full text at.
In Denmark the standard treatment for patients with earlystage cervical carcinoma is RH and pelvic lymphadenectomy. Postmenopausal women undergo bilateral oophorectomy whereas one or both ovaries are preserved in premenopausal women. It was agreed across gynecologic centers to perform a Class IIIII procedure.
Since publication of the last FIGO cervical cancer staging in 2009 considerable progress has been made in the use of imaging modalities to evaluate women with cervical cancer. 2 Although FIGO moved to a surgicopathological system of staging for ovarian and endometrial cancer this was not as simple for cervical cancer a disease mainly of.