General guidance on treating pain For opioids prescribing in chronic pain see Opioid Prescribing for hronic Pain. If a weak opioid is required codeine should be used.
General guidance on treating pain For opioids prescribing in chronic pain see Opioid Prescribing for hronic Pain.
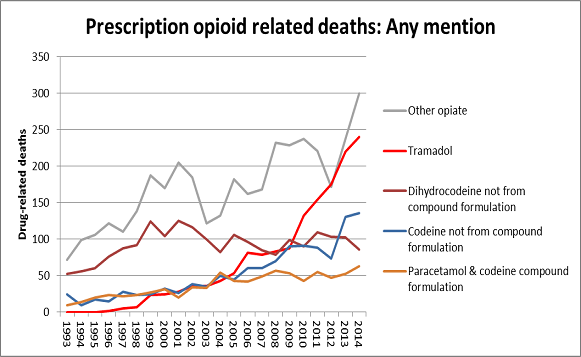
Opioid prescribing guidelines uk. This has been referred to as an opioid epidemic in the UK similar but not at the same scale as the opioid crisis in the USA. The harms of this prescribing are now better understood and government is regulating further. The Medicines and Healthcare products Regulatory Agency will now ensure that packs of opioid medication carry clear warnings about the risks of addiction and dependence.
Where possible the usefulness of opioids should be explored by prescribing a short supply 1-2 weeks of immediate release oral opioid. If a weak opioid is required codeine should be used. If a strong opioid is required immediate release morphine should be used.
No national guidelines on perioperative opioid prescribing. In principle while ensuring the perioperative plan is drawn up in collaboration with the patient and reflects their choices and involvement in their surgical journey all involved health practitioners have the following duties. To ensure that opioids started in the perioperative period are not continued unnecessarily.
When prescribing at the recommendation of another doctor nurse or other healthcare professional you must satisfy yourself that the prescription is needed appropriate for the patient and that prescribing the medicine is within the limits of your competence. Ensure good communication with the patients primary prescriber. The UK General Medical Council advises that clinicians should comply with MHRA recommendations along with other guidance making compliance a professional duty7 Appropriate prescribing of opioids should be a priority focusing where possible on non-pharmacological strategies including referral to wellbeing services physiotherapy exercise and weight loss.
Considerable concern has been raised regarding prescribing rates of opioids in the UK and the awareness of healthcare professionals and patients of the risks of dependence and addiction. Resource for patients and healthcare professionals to support safe prescribing of opioid medicines for pain. It was developed in collaboration with Public Health England the Faculty of Pain Medicine.
This guideline covers safe and effective prescribing of strong opioids for pain relief in adults with advanced and progressive disease. It aims to clarify the clinical pathway for prescribing and help to improve pain management and patient safety. Care during the last 2 to 3 days of life is covered by care of dying adults in the last days of life.
The person who prescribed an opioid or your pharmacist should explain how long it is safe for you to take your medicine for. For further information on using opioids safely and a full list of. General guidance on treating pain For opioids prescribing in chronic pain see Opioid Prescribing for hronic Pain.
Resource pack link Offer non-pharmacological treatments alongside education explanation and reassurance Effervescent preparations should be reserved for patients who cannot swallow. The safe and effective prescribing of strong opioids in adults with advanced and progressive disease is addressed by the NICE guideline on palliative care for adults. Strong opioids for pain relief and is outside the scope of this key therapeutic topic.
Off the back of these reports the National Institute for Health and Care Excellence known as NICE which functions as the health watchdog has decided to create new guidelines for GPs on prescribing opioid painkillers. The guidelines will cover safe prescribing of these drugs and how to manage patients withdrawing from painkillers. Theyre expected to be completed and issued to GPs in.
Do not prescribe more than one type of opioid at a time unless following specialist advice eg. Co-prescription of oral morphine sulphate modified release and transdermal fentanyl. Injectable opioids should never be used as part of a strategy for chronic pain management except in palliative care.
In order to avoid prescribing errors. Prescribe by mass for example 2 mg rather than by volume for example 2 mL. Avoid decimal points in doses if possible for example 25 mg to minimize the risk of dose errors and try to avoid prescribing awkward doses.
Guidelines for Prescribing Opioids in Palliative Care Owner. HDFT Palliative Care Team Author. Dr V Barros DSa Consultant in Palliative Medicine Issue date.
February 2018 Review date. February 2020 Ratified and approved by. Area Prescribing Committee On.
Responsibility for prescribing opioids Whilst tapering opioids the patient should ideally receive prescriptions from a single prescriber and the medicine dispensed from a specified pharmacist. Onsider using the home screen of the medical record to highlight. Methadone oral solution 1 mgmL is the recommended choice it is licensed for the treatment of opioid dependence in the UK.
Other strengths for example 10 mgmL or 20 mgmL may rarely be prescribed in specialist settings to people on high-dose methadone but these should normally be on a supervised consumption basis because. OPIOID PRESCRIBING FOR ACUTE PAIN KEY RECOMMENDATIONS GOAL The goal for prescribing opioids in acute pain should be a tolerable level of pain that facilitates optimal physical and emotional function and avoidance of complications. 1 BEFORE PRESCRIBING OPIOIDS Undertake comprehensive assessment.
Promote and optimise non-pharmacological. In view of the opioid crisis that is beginning to be seen in the UK 8 we need to avoid the use of modified release opioid preparations for acute pain which is in line with US and antipodean recommendations 9 we need to avoid opioids prescribed for acute pain continuing on to repeat prescriptions and we need to limit the size and duration of our prescriptions. 9 PRESCRIBING GUIDANCE IN SUBSTANCE MISUSE SERVICES_PHA46_MAY 2019 55 Initiating Methadone Prescribing 551 The decision to initiate opioid substitute prescribing on an outpatient basis is made following multi-disciplinary assessment and the development of a treatment and.