
02 to 30 mUL. Overt thyroid disease in pregnancy is associated with several negative outcomes.
Many symptoms of hypothyroidism are similar to pregnancy symptoms.
Hypothyroidism third trimester pregnancy. How hypothyroidism affects mid and late-stage pregnancy During second and third trimester of pregnancy all of the fetuss organs will rapidly develop in preparation for birth. Thyroid glands of both the mother and fetus play a major role in all the developmental stages and its necessary to make sure the thyroid and immune system are properly functioning during these stages. Within a joint endocrine-obstetric clinic maternal hypothyroidism at presentation and in the third trimester may increase the risk of low birthweight and the likelihood for caesarean section.
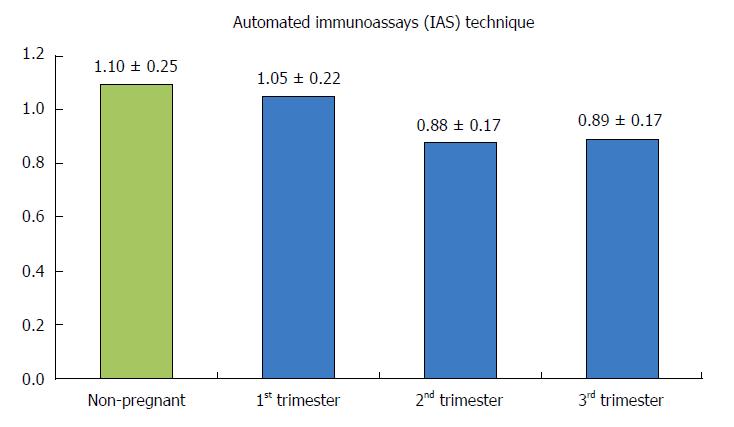
The latter observation was not due to a higher rate of emergency caesarean section nor to a lower threshold for performing elective caesarean section. Hypothyroidism can occur during pregnancy due to the initial presentation of Hashimotos thyroiditis inadequate treatment of a woman already known to have hypothyroidism from a variety of causes or over-treatment of a hyperthyroid woman with anti-thyroid medications. Serum TSH levels decrease in the first trimester and increase in the second and third trimesters.
However not to prepregnancy levels. Hypothyroidism is present in up to 3 of all pregnant women. Maternal thyroid volume increases 10-30 in pregnancy especially in 3 rd trimester as a result of increased blood volume and extracellular fluid.
An enlarged thyroid gland in isolation is not an indication for screening for thyroid disease if no other clinically relevant history symptoms or. Hypothyroidism is a condition marked by an underactive thyroid gland and may be present during pregnancy. Many symptoms of hypothyroidism are similar to pregnancy symptoms.
For example fatigue weight gain and abnormal menstruation are common to both. Hypothyroidism is a deficiency of the thyroid hormone thyroxine due to an underactive thyroid gland. During pregnancy the condition which occurs in about two to three of every 500 expecting women is usually caused by Hashimotos disease an autoimmune disorder that causes chronic inflammation of the thyroid gland and interferes with its ability to produce hormones.
Standard TSH levels during Pregnancy. 01 to 25 mUL. 02 to 30 mUL.
02 to 30 mUL. These reference ranges are for the thyroid lab test TSH which we will discuss more below and they are considered to be tighter when compared to healthy people and women who are not pregnant. Among women who had at least one adjustment in thyroid hormone dosage during gestation the median cumulative increase in levothyroxine from preconception to third trimester was 44 consistent with previously published data 5 9.
The cohort in this study included pregnancies between 2014 and 2017. Read the article and chart of thyroid levels during pregnancy. Chart of normal thyroid TSH levels during first second and third trimester of pregnancy.
The normal range of TSH levels is 035 to 50 mIULiter. Hypothyroidism in pregnancy is usually caused by Hashimotos disease and occurs in 2 to 3 out of every 100 pregnancies. 1 Hashimotos disease is an autoimmune disorder.
In Hashimotos disease the immune system makes antibodies that attack the thyroid causing inflammation and damage that make it less able to make thyroid hormones. Hypothyroid states should be treated with thyroxine aiming for a TSH. Thyroxine should be increased by two additional doses per week or 30 on suspicion or confirmation of.
Overt thyroid disease in pregnancy is associated with several negative outcomes. Untreated overt hypothyroidism can result in preterm birth low birth weight miscarriage stillbirth placental abruption preeclampsia heart failure and impaired neurocognitive development 3. The reference interval of thyroidstimulating hormone in the 25th and 975th percentiles has a significant increasing trend from the first trimester to second trimester and to third trimester which was 008379 mIUL for the first trimester and 012395 mIUL for the second trimester and 038418 mIUL for the third trimester.
Serum total T4 and total T3 steadily increase during pregnancy to approximately 15 times the non-pregnant level by mid second trimester 3-6. Whereas serum free T4 and free T3 gradually decrease during pregnancy 47. While the values for most thyroid function tests generally lie within normal non-pregnant ranges.
In fact less than 2 percent of babies born to mamas with Graves disease suffer from hyperthyroidism themselves. Still baby will need to be tested right after birth just in case. Signs of hyperthyroidism in baby include an increased fetal heart rate enlargement of the fetal thyroid gland and poor growth of the fetus.
Disease during pregnancy are at higher risk of developing very severe hyperthyroidism known as thyroid storm. Graves disease often improves during the third trimester of pregnancy and may worsen during the post partum period.