There are many different types of HPV and some are more likely than others to lead to cervical cancer. These include commercial tests.
With these National HIV Testing and Treatment Guidelines - 2017 our traditional facility-based HIV testing in clinical settings such as standalone HIV testing services and antiretroviral therapy sites mobile facilities antenatal care and labour rooms opioid substitution therapy sites TB care sites and private clinics have been expanded.
Hpv testing guidelines 2017. Results The major recommendations include 1 testing newly diagnosed oropharyngeal squamous cell carcinoma patients for high-risk HPV either from the primary tumor or from cervical nodal metastases using p16 immunohistochemistry with a 70 nuclear and cytoplasmic staining cutoff and 2 not routinely testing nonsquamous oropharyngeal carcinomas or nonoropharyngeal carcinomas for. Updated to provide additional guidance on the use of IQC material and advice on training and competency requirements for staff using a new HPV platform. ACS recommends cervical cancer screening with an HPV test alone every 5 years for everyone with a cervix from age 25 until age 65.
If HPV testing alone is not available people can get screened with an HPVPap cotest every 5 years or a Pap test every 3 years. Those aged 25 to 65 should have a primary HPV test every 5 years. If primary HPV testing is not available screening may be done with either a co-test that combines an HPV test with a Papanicolaou Pap test every 5 years or a Pap test alone every 3 years.
A primary HPV test is an HPV test that is done by itself for screening. The US Food and Drug Administration has approved certain tests to be primary HPV tests. After a successful evaluation of the feasibility of HPV-based screening in 2014 primary HPV testing for cervical screening was implemented in 2017.
The Netherlands has been one of the first countries worldwide to implement nationwide HPV-based screening and its experience with the new programme is therefore followed with great interest. In this manuscript we present an overview of the studies that were instrumental in the choice of HPV. Women ages 21 through 29 should be screened with a Pap test every 3 years.
Women ages 30 through 65 should be screened with any of three tests. Every 5 years with high-risk HPV testing alone. Every 5 years with Pap and high-risk HPV cotesting.
Every 3 years with a Pap test alone. With these National HIV Testing and Treatment Guidelines - 2017 our traditional facility-based HIV testing in clinical settings such as standalone HIV testing services and antiretroviral therapy sites mobile facilities antenatal care and labour rooms opioid substitution therapy sites TB care sites and private clinics have been expanded. This include innovative public-private.
Based on these changes in practice the need to interpret HPV test results is a common issue for clinicians. There are many potential combinations of cervical cytology and HPV results and some of these combinations or serial testing results are not addressed by guidelines. In addition some laboratories offer tests that are not included in screening guidelines.
These include commercial tests. Primary HPV testing for average-risk asymptomatic women 30years old was recommended by 408 of physicians who performed cervical cancer screening and 901 of these providers recommended primary HPV testing for women of all ages. Drafted guidelines to promote primary HPV testing and eliminate a cotesting option in 2017 but efforts from sev-eral professional societies led to changes in the final 2018 guidelines to allow for continued cotesting6 The second major change in the 2020 ACS guide- line in comparison with the 2012 version is that the recommended age to initiate screening is 25 years for average-risk.
Revised Recommendations for HIV Testing of Adults Adolescents and Pregnant Women in Health Care Settings. Provides recommendations on routine opt-out HIV screening of adults adolescents and pregnant women in health care settings in the United States. This HPV primary screening implementation guidance includes information on.
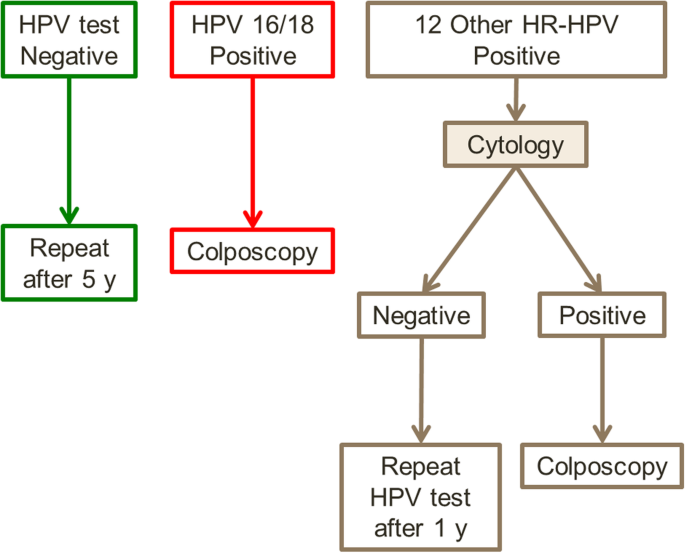
Testing every two years25 From December 2017 in the renewed NCSP it will be recom-mended that women aged 2574 years attend for primary HPV testing every five years with partial genotyping for HPV 16 and 18 and liquid based cytology LBC triage for women in whom oncogenic HPV not 1618 is detected. Women in whom HPV 1618 is. Guidelines on HIV self-testing and partner notification.
Supplement to consolidated guidelines on HIV testing services Page ii Acknowledgements The development of this document would not have been possible without the help of the organizations that submitted case examples and the amazing people working with them. The new screening method will test for the presence of human papillomavirus HPV. About four out of five people have an HPV infection at some time in their lives.
There are many different types of HPV and some are more likely than others to lead to cervical cancer. For most people an HPV infection clears by itself within two years especially in people under 30. You might not even know youve had.
We revised the clinical follow up schedule to include STI testing for asymptomatic MSM at high risk for recurrent STIs eg those with recent STIs or multiple sex partners at the 3 month visit in addition to testing for all symptomatic sexually-active persons. This is consistent with 2015 STD guidelines. The major recommendations include 1 testing newly diagnosed oropharyngeal squamous cell carcinoma patients for high-risk HPV either from the primary tumor or from cervical nodal metastases using p16 immunohistochemistry with a 70 nuclear and cytoplasmic staining cutoff and 2 not routinely testing nonsquamous oropharyngeal carcinomas or nonoropharyngeal.
VC 2017 American Cancer Society. Aptima human papillomavirus HPV test. High-grade squamous intraepi- thelial lesion HSIL.
HPV E6E7 messenger RNA test. INTRODUCTION In the past 2 decades significant advances in the prevention and treatment of cervical cancer have been achieved. Part of this effort the first counselling and testing guidelines were published by the federal Ministry of Health FMOH in 1996 and the second edition currently in use in 2002.
Rapid expansion of the ART program provided an unprecedented opportunity to rapidly scale up HIVAIDS prevention care and treatment services in Ethiopia. To guide this movement the government with partners.