
4 as in other druginduced pulmonary reactions regression may follow steroid administration. Amiodarone can cause numerous kinds of lung problems but in most cases the problem takes one of four forms.
The pulmonary toxicity associated with amiodarone therapy is clinically complex and likely reflects underlying mechanisms of lung injury that result from direct toxic effects of the drug or its metabolites as well as indirect inflammatory and immunologic processes induced by the drug therapy.
Amiodarone pulmonary toxicity mechanism. The onset of pulmonary toxicity may be either insidious or rapidly progressive. Cough new chest infiltrates in imaging studies and reduced lung diffusing capacity in the appropriate clinical setting of amiodarone use after the meticulous exclusion of infection malignancy and pulmonary oedema are the cardinal clinical and laboratory elements for diagnosis. The pulmonary toxicity associated with amiodarone therapy is clinically complex and likely reflects underlying mechanisms of lung injury that result from direct toxic effects of the drug or its metabolites as well as indirect inflammatory and immunologic processes induced by the drug therapy.
A Mechanistic Study on the Amiodarone-Induced Pulmonary Toxicity 1. Amiodarone AM is benzofuran derivative with highly effective class III antidysrhythmic activity. Amiodarone was obtained from MP Biomedical USA.
Amiodarone has been implicated in pulmonary toxicity even though there is no direct link because 1 no other cause could be found for the reactions that occurred. 2 radiographic lesions cleared when amiodarone was discontinued or the dose reduced. 3 lung biopsies revealed changes similar to those seen in other drug reactions.
4 as in other druginduced pulmonary reactions regression may follow steroid administration. And 5 specific therapy for other possible pulmonary. The mechanism of amiodarone pulmonary toxicity is unknown and recommendations for the assessment and treatment of patients with this condition continue to evolve.
In two patients with clinically diagnosed amiodarone pulmonary toxicity a rapidly progressive and fatal adult respiratory distress syndrome developed after pulmonary angiography. A known complication of Amiodarone therapy is Amiodarone induced Pulmonary Toxicity APT. Several features of this adverse effect make it difficult to diagnosis and treat.
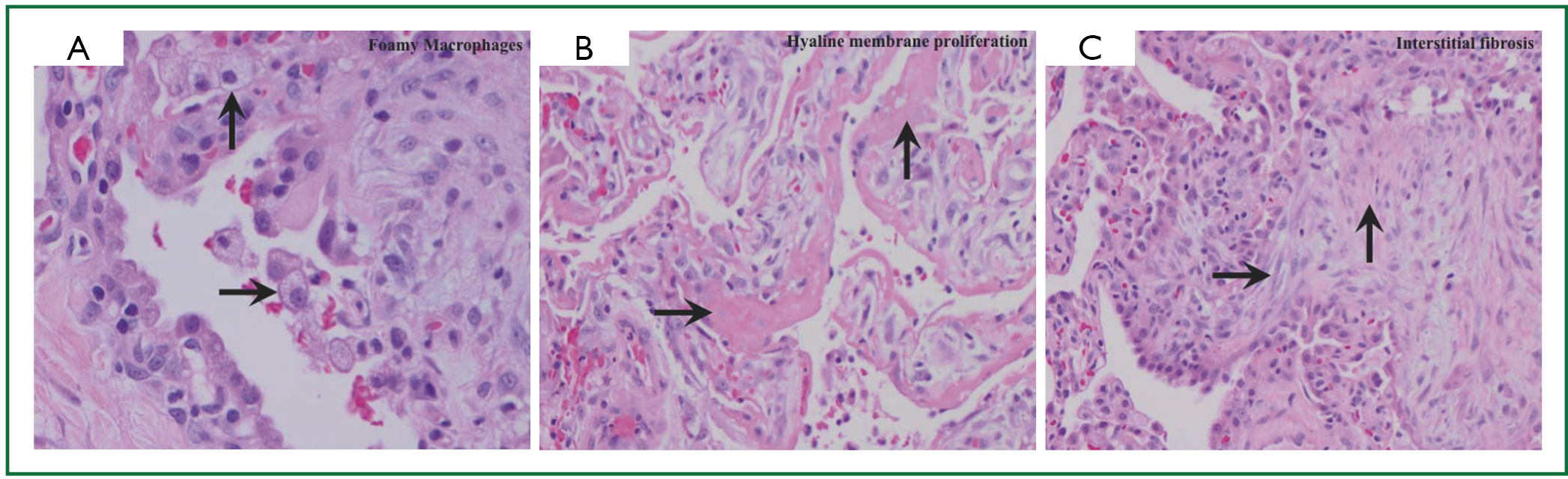
The case of a 63-year-old male with classic radiographic and histologic findings of APT is discussed. Amiodarone- induced pulmonary toxicity AIPT is characterized in part by oedema phospholipidosis inammation and thickening of the alveolar septa intra-alveolar inammation and pul- monary brosis. E etiology of AIPT is unknown.
Howeverseveralcauseshavebeenproposedincludingdirect or indirect toxicity. To determine possible mechanisms this study utilizes a unique in vitro cell culture model of amiodarone pulmonary toxicity and demonstrates that amiodarone can directly induce an accumulation of phospholipids within bovine pulmonary artery endothelial BPAE cells during the first 24 hr using amiodarone concentrations equivalent to concentrations found in the blood and lungs of human subjects. The mechanism of amiodarone-induced pulmonary toxicity is not entirely clear but is thought to be caused by direct cytotoxic damage and an indirect immune reaction.
Amiodarone inhibits phospholipase A which can result in an accumulation of phospholipids within lysosomes in. Amiodarone lung toxicity probably affects up to 5 of patients taking this drug. It is not known whether the lung problems caused by amiodarone are due to direct damage by the drug to the lungs tissues to an immune reaction to the drug or to some other mechanism.
Amiodarone can cause numerous kinds of lung problems but in most cases the problem takes one of four forms. Amiodarone is an iodine-containing antiarrhythmic drug commonly used for the treatment of ventricular and supraventricular arrhythmias. Amiodarone toxicity has several clinical presentations and affects multiple organs.
One well-known serious side effect of amiodarone is pulmonary toxicity which can be acute sub-acute or chronic. Although none of the available information identifies the mechanism mediating amiodarone pulmonary toxicity the frequency of the complication probably can be reduced by timely reductions in. Amiodarone-induced pulmonary toxicity can present acutely hours to days after surgery or angiography or chronically months to years after starting amiodarone treatment.
Acute toxicity eg acute respiratory distress syndrome is rare but is associated with high mortality up to 50. Chronic toxicity eg chronic interstitial pneumonitis. APTamiodarone pulmonary toxicity A miodarone long used for various arrhythmias has been associated with a long list of side effects.
Amio darone pulmona1y toxicity APT was first reported in 19801 It occurs in 5 to 10 of tr eated pati nts and is one of the more serious complications seen with amiodarone. Because amiodarone is a cytochrome P450 inhibitor simultaneous administration of other drugs should be considered carefully to minimize the risk of interactions. Primary mechanism of action.
Antiarrhythmic effect via blockage of voltage-gated potassium channels prolonged repolarization of the cardiac action potential.